Like most industries, healthcare is swiftly evolving to adopt real-time monitoring technologies. The field of remote patient monitoring (RPM) has rapidly expanded to fight COVID-19 and will impact healthcare far beyond the pandemic. With the removal of reimbursement barriers, the advancement of telecommunications technology, and a growing need for healthcare access, RPM technology markets will double in the next five years.
What You Need to Know About RPM
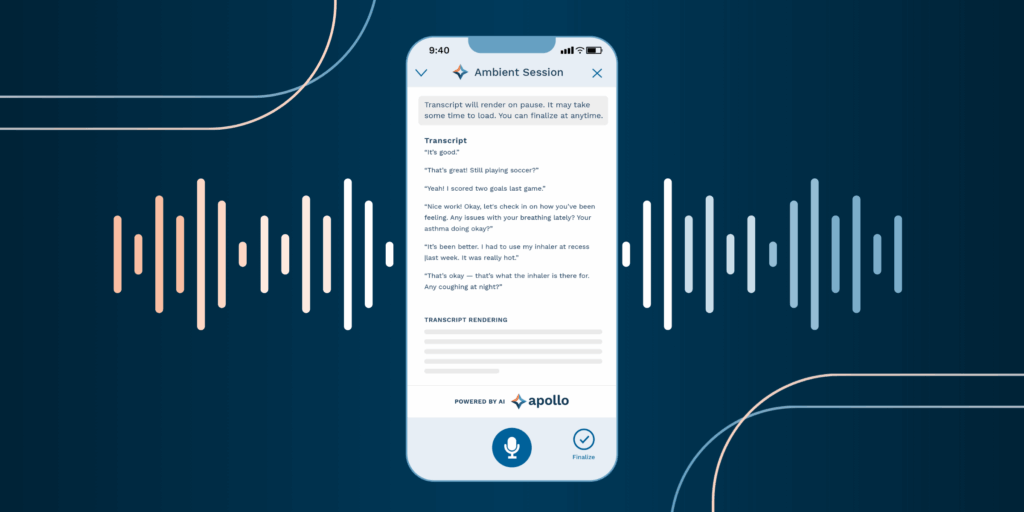
RPM uses digital, often cloud-based, technology to acquire, process, and transmit health data. The most well-known form of health monitoring is telehealth or telemedicine, which includes videoconferencing, virtual appointments, mobile messaging, and both clinical and non-clinical services, etc. Meanwhile, a growing area of RPM is mobile phone sensing systems, such as vital sign readings, fall monitoring systems, and applications to monitor chronically ill patients.
What started as relatively simple applications to monitor patients in hospitals have developed much further so patients can perform daily activities, exercises, and health plans from the comfort of their homes. Electronic patient health data is monitored and securely transmitted to healthcare providers in different locations for assessment and recommendations from this remotely acquired data.
RPM has many advantages including:
- Early and real-time illness detection
- Reduction of healthcare costs
- Constant monitoring
- Chronic disease management
- Prevention of worsening of illnesses and untimely deaths
- Reduction of hospital admissions and emergencies
Highly vulnerable patients are among those who stand to gain the most from remote monitoring. Health monitoring has shown to be significantly useful and far less costly for patients with mobility issues located in rural areas, in critical emergency care, and those who are socioeconomically disadvantaged.
Remote Patient Monitoring in the Pandemic
During the COVID-19 pandemic, RPM allowed providers to monitor patients without coming into contact with them, mitigating the virus’s spread and preserving critical hospital space for severe cases.
The Mayo Clinic’s remote patient monitoring program has been one of the most successful COVID-19 RPM care cases. Two tracks have been developed to monitor patients: one for higher-risk patients with comorbidities and one for those at lower-risk. Patients are monitored 24/7 to assess any changes in their biometric data, with goals to detect any significant changes in the patients’ vitals as early as possible.
The RPM program led to decreased exposure to COVID-19 for providers, other patients, and medical staff. It has also increased critical hospital capacity, reduced time in the hospital, and reduced patient costs when many are struggling financially.
These benefits have far outweighed any technology adoption latencies. “We thought we’d have more technical issues, but the technology is easy to use and work with,” said Ravindra Ganesh, M.B.B.S., M.D., an internal medicine physician and director of the COVID-19 Front-Line Care Team in the Midwest. Even geriatric patients who tend to be latent technology adopters can navigate care with wearable technology developments.
The Future of Remote Health Monitoring
Continued demand for telemedicine will drive improved RPM devices, while accurate remote diagnosis and monitoring systems will be necessary to collect vital signs and other data points. As new wearable and multi-sensor technology emerges, smart device integrations with clinical EHRs will optimize day-to-day operations and provide data for strategic decision-making.
Wearable devices such as wristbands, smartwatches, wearable mobile sensors, and other medical devices that collect a range of data (blood sugar, exercise routines, sleep, etc.) have the potential to transform patient care. According to the Pew Research Center, 60% of US adults already report tracking their weight, diet, or exercise routines, with 33% of US adults tracking health symptoms or indicators such as blood pressure, blood sugar, or sleep patterns. Increased use and interoperability of these devices can help patients monitor their own health data from anywhere. They will also allow patients and providers to manage chronic conditions such as diabetes, heart conditions, and chronic pain as well as engage in personalized, predictive care.
Enhance Adoption with Patient-Centric Digital Systems
As telehealth services and remote patient monitoring systems expand, providers must move toward streamlined digital patient experiences. With well-integrated electronic health record and practice management software systems, practices of all sizes and specialties can streamline record management processes and transfer health data, and communicate with patients and other professionals more easily.
Customizable patient interactions, convenient lab orders and results, integrated patient portals, easier patient check-in, and seamless connections and data exchanges are all user-friendly digital experiences that will aid adoption and seamless integration into a shifting healthcare landscape.
Learn more about RXNT’s cloud-based EHR software and how it can improve patient outcomes, streamline your practice, and support providers’ access to critical data.